Back pain constitutes one of the most common non-emergent medical complaints: for example, it is estimated that around 80 percent of Americans will experience chronic back pain within their lifetime.1 Despite the prevalence of back pain, it can be immensely difficult to treat; thus, preventative medicine remains the most effective approach. A number of factors can contribute to back pain, including occupation, age, and ergonomics. Perhaps one of the most pertinent contributing factors is body mass index. Ever since a 2010 study by Shiri et al. showed a direct correlation between obesity and back pain,2 it has been well-established that being overweight is highly associated with back pain. At first glance, this finding may not seem surprising: after all, increased weight places greater strain on the musculoskeletal structure, including the muscles and joints of the spine. Yet some debate remains as to whether the association can be explained so simply.
For example, in 2017, researchers at Cornell initiated an investigation to establish which specific back pain-causing conditions were associated with being overweight. Their findings were surprising: obesity was a predictor of only two of the four conditions studied, which were lower back pain and internal disc disruption.3 Spine degeneration (otherwise known as spondylosis) and neck problems were found to be unrelated to obesity. These results would suggest that other factors outside of body weight and mechanics are involved. Other studies, such as a 2015 one performed by Dafina Ibrahimi-Kaçuri et al., have shown that obesity may simply aggravate preexisting conditions instead of causing new ones.4 In fact, the authors concluded: “Obesity and age have no direct influence in back pain, but they could prolong healing.”4 Instead, they argue, factors such as physical workload are more likely to be the direct cause of chronic back pain.
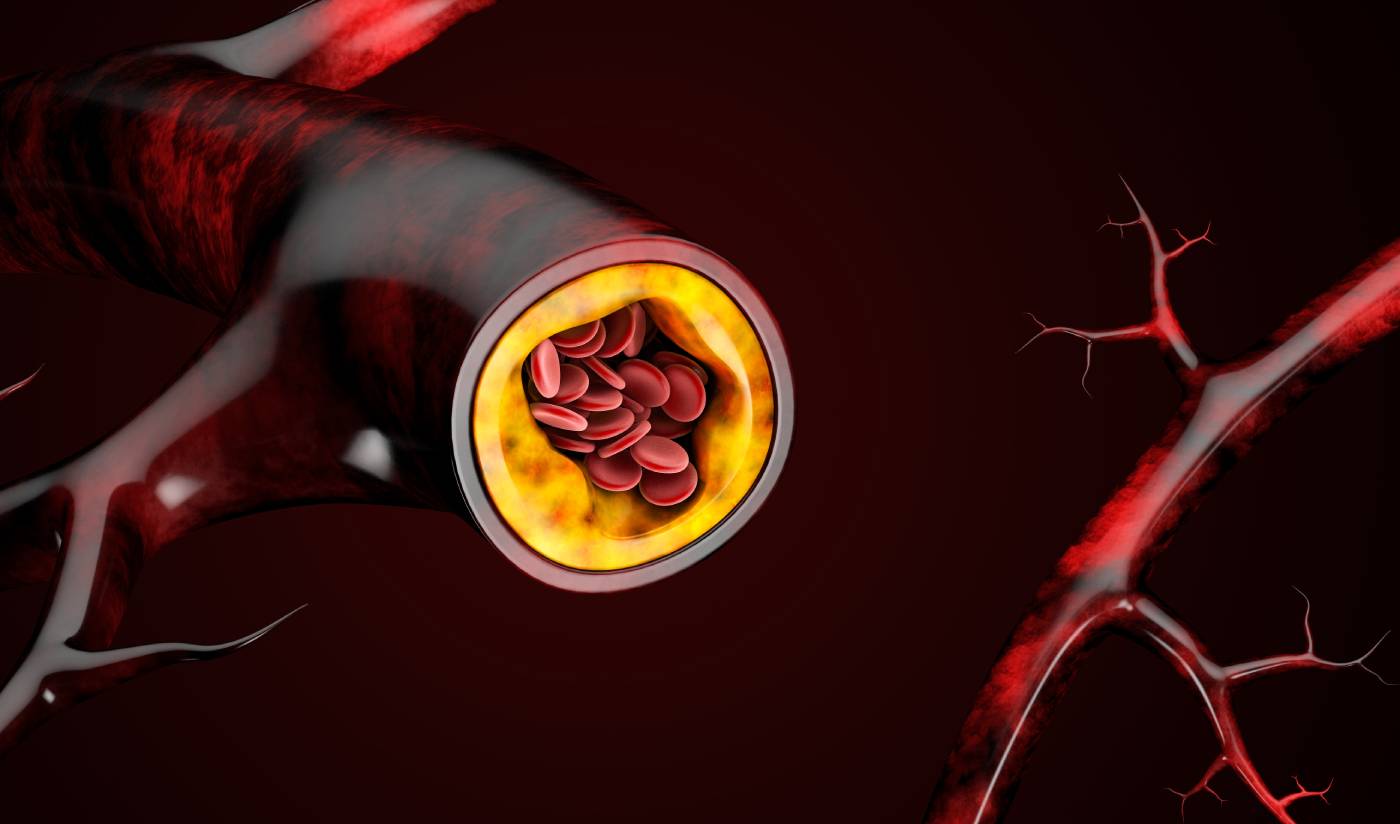
On the other hand, it is clear that obesity can substantially alter normal bodily mechanics, which in turn places undue strain on one’s back. For example, a cross-sectional study of obese women demonstrated that having increased weight in the lower abdomen changed individuals’ centers of gravity, shifting their pelvis forward and straining the vertebrae inward (a condition called hyperlordosis).5 Such drastic shifts in alignment could, over time, cause chronic pain. Moreover, researchers have also suggested that adipose tissue itself might trigger metabolic shifts, which may play as much a part in back pain as the physical burden of additional weight.6 It is thought that these accumulative factors may explain why individuals who are obese are highly susceptible to herniated discs and sciatica, as well as lumbar radicular pain.
While it remains unclear whether obesity is a cause or simply an aggravating factor when it comes to chronic back pain, there is little doubt that having a normal body weight can help in the avoidance of severe back pain. This is therefore a factor that should be taken into consideration when it comes to the treatment of this common issue. Healthcare providers might therefore consider incorporating healthy lifestyle and weight loss plans into their treatment regimens for the management of chronic back pain in obese patients.
References
1. Urits, I., Burshtein, A., Sharma, M., Testa, L., Gold, P. A., Orhurhu, V., Viswanath, O., Jones, M. R., Sidransky, M. A., Spektor, B., & Kaye, A. D. (2019). Low Back Pain, a Comprehensive Review: Pathophysiology, Diagnosis, and Treatment. Current Pain and Headache Reports, 23(3), 23. https://doi.org/10.1007/s11916-019-0757-1
2. Shiri, R., Karppinen, J., Leino-Arjas, P., Solovieva, S., & Viikari-Juntura, E. (2010). The association between obesity and low back pain: a meta-analysis. American Journal of Epidemiology, 171(2), 135–154. https://doi.org/10.1093/aje/kwp356
3. Sheng, B., Feng, C., Zhang, D., Spitler, H., & Shi, L. (2017). Associations between Obesity and Spinal Diseases: A Medical Expenditure Panel Study Analysis. International Journal of Environmental Research and Public Health, 14(2), 183. https://doi.org/10.3390/ijerph14020183
4. Ibrahimi-Kaçuri, D., Murtezani, A., Rrecaj, S., Martinaj, M., & Haxhiu, B. (2015). Low back pain and obesity. Medical Archives (Sarajevo, Bosnia and Herzegovina), 69(2), 114–116. https://doi.org/10.5455/medarh.2015.69.114-116
5. Vismara, L., Menegoni, F., Zaina, F., Galli, M., Negrini, S., & Capodaglio, P. (2010). Effect of obesity and low back pain on spinal mobility: a cross sectional study in women. Journal of Neuroengineering and Rehabilitation, 7, 3. https://doi.org/10.1186/1743-0003-7-3
6. Rosen, E. D., & Spiegelman, B. M. (2014). What we talk about when we talk about fat. Cell, 156(1-2), 20–44. https://doi.org/10.1016/j.cell.2013.12.012