Age Considerations for Chiropractic Care
Unique considerations need to be made with regard to health as individuals navigate life. The needs of babies are vastly different from the needs of older adults, and chiropractors need to take into account these developmental differences when treating patients. Patient-tailored chiropractic care that takes age into account can benefit a wide range of patients at all stages of life.
Young infants undergo many changes very swiftly, and chiropractors can play a role in their health and correcting certain conditions. In particular, chiropractors can help address musculoskeletal abnormalities or other issues such as torticollis 1.
As they grow, children may experience injuries or development that can be treated through chiropractic care that is appropriate for their age. Chiropractors have indeed been treating children for many years, and child chiropractic care is very safe. Studies that assess malpractice insurance coverage have demonstrated an exceptional safety record. Chiropractic adjustments can treat infants and children despite their young age. Chiropractic care can even help women prior to childbirth by aligning her spine and pelvis 2.
Adolescents undergo significant pressure as their bodies change rapidly throughout adolescence. First, chiropractors can help adolescents with the rehabilitation they need for injuries sustained during sports and other activities. In addition, chiropractors can support adolescents with stress and anxiety management while teaching them how to nourish healthy and sustainable lifelong habits.
Adults can greatly benefit from regular, individualized chiropractic care and make up the greatest subset of chiropractic patients. A chiropractor will assess a patient’s life and physical condition, while monitoring a patient’s posture and physical features, in order to craft the best possible care regimen for a patient. For example, adults often experience more health problems with age, and chiropractic care should adjust based on an individual’s needs. The chiropractor to this end can make specific recommendations, perform patient-tailored treatments, and help patients lead a smooth, healthy life.
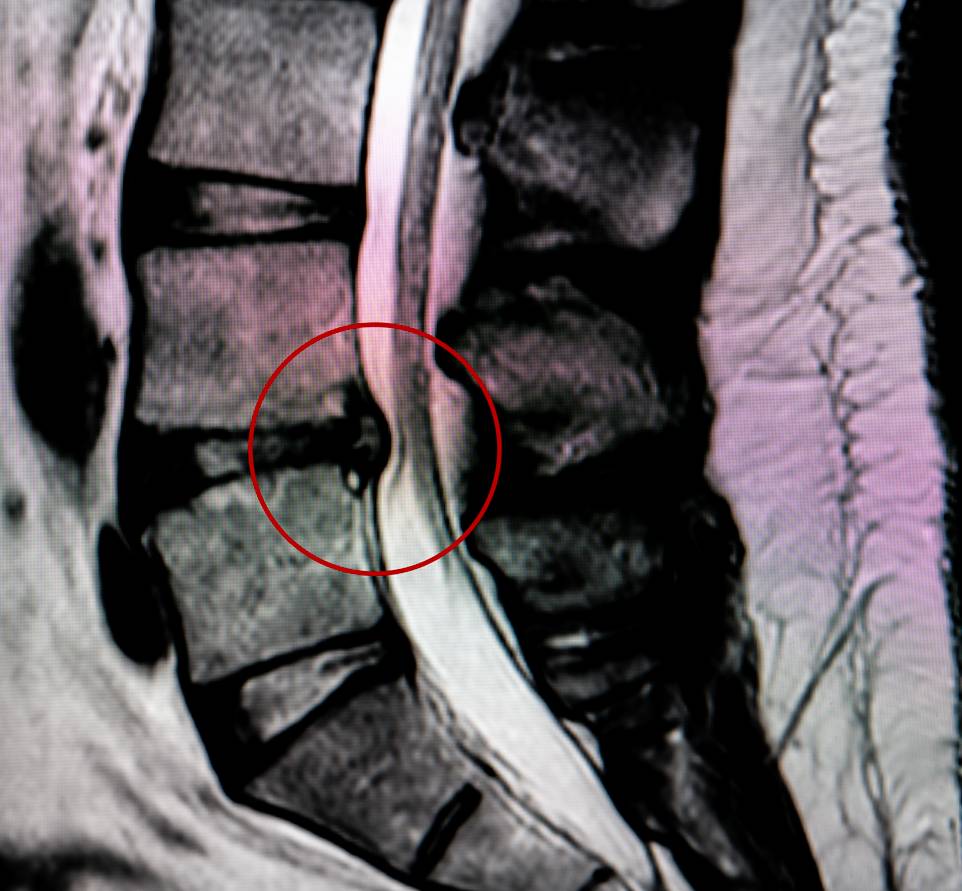
Aging can be very difficult on one’s body. First, chiropractic care can reduce the pain associated with the very frequent age-related spine changes. In addition, chiropractic care can help alleviate the challenges associated with a host of other musculoskeletal issues. A recent study showed that among a cohort of adults over 65 years of age, nearly 60% suffered from back issues, with neck pain and lower limb issues being the next most common presentations to chiropractors. However, additional research is warranted to better explore the clinical course of back pain in older patients seeking chiropractic care and compare the different ways of providing care to them across healthcare professions 3.
Overall, like for infants and children, the provision of chiropractic care in older adults is very safe. Research focused on the safety of chiropractic care revealed the importance of chiropractors advising patients on exercise and implementing manipulation and mobilization protocols that contribute to general positive outcomes, well beyond pain reduction exclusively 4. Such targeted chiropractic care will ensure that seniors age as gracefully as possible, living a healthy, comfortable life.
References
1. Chiropractic Care for Every Age: What You Should Know – Awaken Chiropractic & Sports Medicine. Available at: https://awakenchiroco.com/chiropractic-care-for-every-age-what-you-should-know/. (Accessed: 7th January 2024)
2. What Age Should You Begin Chiropractic? Available at: https://irvingtxchiro.com/what-age-should-you-begin-chiropractic/. (Accessed: 7th January 2024)
3. de Luca, K., Hogg-Johnson, S., Funabashi, M., Mior, S. & French, S. D. The profile of older adults seeking chiropractic care: a secondary analysis. BMC Geriatr. 21, (2021). doi: 10.1186/s12877-021-02218-6.
4. Hawk, C. et al. Best Practices for Chiropractic Care for Older Adults: A Systematic Review and Consensus Update. J. Manipulative Physiol. Ther. 40, 217–229 (2017). doi: 10.1016/j.jmpt.2017.02.001.