Prognosis for Herniated Disc
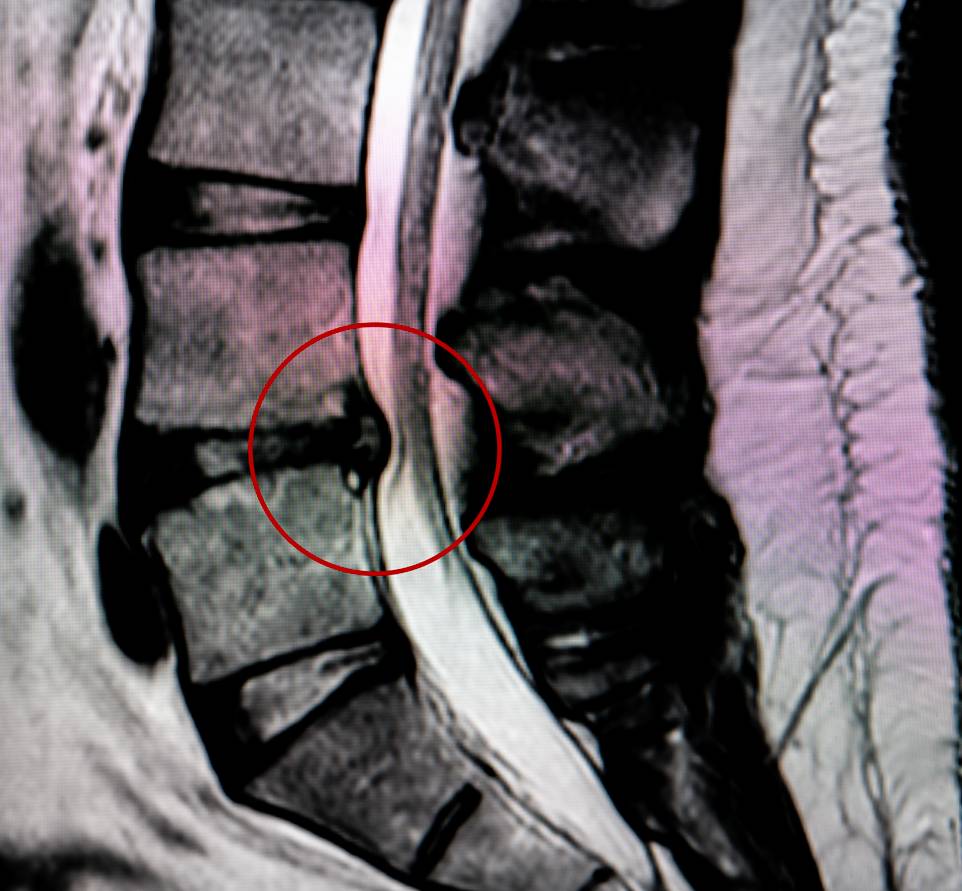
The prognosis of a herniated disc, a prevalent spine illness, is a major focus of medical research. Initial pain is frequently followed by progressive radiculopathy, which can impact daily life and function. Lumbar disc herniation, which affects 2-3% of the population, normally goes away in four to six weeks. The suggested initial treatment consists of conservative treatments such as medicine, physiotherapy, and, in certain cases, percutaneous nerve root block. Because the condition is benign, treatment focuses on pain relief and neurological recovery, encouraging a prompt return to daily activities and work. For many patients, the prognosis after a herniated disc is positive and includes significant recovery.
Because of their anti-inflammatory properties, NSAIDs are the preferred medication with a positive prognosis for herniated disc, particularly when supplemented by analgesics. Conservative treatment is most beneficial for young patients with small, sequestered hernias, mild neurological deficits, and minimal disc degeneration. Sciatica has a natural history of rapid symptom relief over four to six weeks, with recurrences occurring in approximately 5 to 10% of cases, regardless of treatment type. Surgical treatment is indicated for sciatica that has been unresponsive to conservative treatment for six weeks or more, significant motor deficits, or sciatica with foraminal bone stenosis. In cases of insufficient pain control, significant motor deficit (grade 3 or higher), radicular pain with foraminal stenosis, or cauda equina syndrome, surgical intervention is required. A refined surgical approach entails removing the extruded fragment while preserving the ligamentum flavum, addressing sciatic symptoms, and lowering the risk of long-term recurrence. [1]
The findings of Moranjkiv et al. shed more light on the variables influencing the prognosis after surgery for a lumbar herniated disc. Their research indicates that several factors, including age, pain duration and intensity, and the specific type of disc herniation are important indicators of how well a surgery will go. Gender has no effect on these outcomes, which is surprising since other studies have cited a predisposition among males. They also discovered that patients who work sedentary jobs and have no motor or sensory deficits have better post-surgery outcomes. The presence of intraoperative complications such as dural tears or root damage, on the other hand, is associated with a worse prognosis. Notably, leg pain that lasts more than eight months prior to surgery is associated with poorer outcomes, including a higher risk of not returning to work. [2]
Wong et al. concentrate on cervical spine disc herniation, a common cause of cervical radiculopathy. Risk factors such as male gender, smoking, heavy lifting, and certain occupations are included in the prognosis. Most patients have severe neck and arm pain, as well as sensory and motor symptoms. Conservative care is recommended at first, with surgery considered if pain persists after 6 to 12 weeks or if motor deficits progress. According to their systematic review, the prognosis of cervical disc herniations with radiculopathy is generally favorable, with significant improvements occurring within 4 to 6 months and full recovery taking 24 to 36 months. Furthermore, Wong et al. claim that the early clinical course of cervical disc herniations is similar to that of lumbar disc herniations, with significant improvements seen in the first 6 to 12 months after treatment.
However, due to the limited scope of current research, the prognosis for cervical herniated disc is less clear, particularly in terms of recurrent episodes and long-term outcomes. For example, a small percentage of patients may have residual impairments such as pain and activity limitations. The need to file workers’ compensation claims has been identified as a prognosis factor associated with poorer outcomes as well. [3] Considering different clinical, surgical, and demographic factors is crucial when determining the prognosis of spinal disc herniations, as these studies collectively demonstrate.
References
1. Vialle, Luis Roberto et al. “Lumbar Disc Herniation.” Revista brasileira de ortopedia vol. 45,1 17-22. 16 Nov. 2015, doi:10.1016/S2255-4971(15)30211-1
2. Moranjkic, Mirza et al. “Outcome Prediction in Lumbar Disc Herniation Surgery.” Acta Medica Saliniana vol. 39, 2 75-80. 17 Feb. 2010, doi:10.5457/ams.103.09
3. Wong, Jessica J et al. “The course and prognostic factors of symptomatic cervical disc herniation with radiculopathy: a systematic review of the literature.” The spine journal : official journal of the North American Spine Society vol. 14,8 (2014): 1781-9. doi:10.1016/j.spinee.2014.02.032