How Chiropractors Treat Sacroiliac Joint Pain
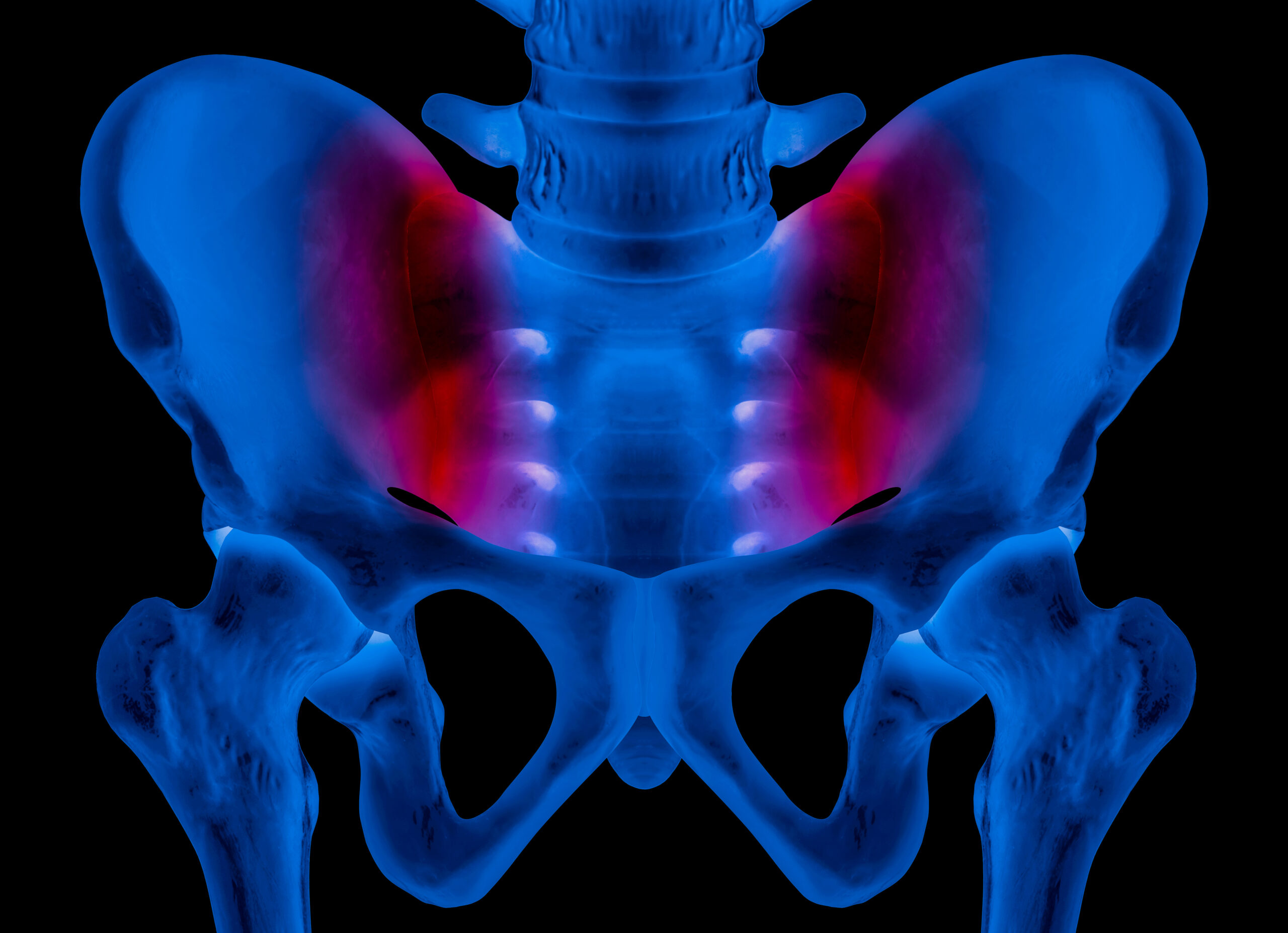
Sacroiliac joint pain is a common condition that affects many individuals, causing discomfort and limiting mobility. Chiropractors are experts in treating musculoskeletal disorders, and they have several techniques to address sacroiliac joint pain.
Sacroiliac joint pain can be caused by various factors, including arthritis, injury, pregnancy, or prolonged sitting. The symptoms may include lower back pain, hip pain, leg pain, and difficulty standing or sitting. The chiropractor’s goal is to relieve the pain, improve mobility, and restore the normal function of the joint.
The first step in treating sacroiliac joint pain is to diagnose the cause of the condition accurately. The chiropractor will conduct a thorough physical exam, including a review of the patient’s medical history and imaging tests if necessary. Once the diagnosis is established, the chiropractor will design a personalized treatment plan that may include one or more of the following techniques.
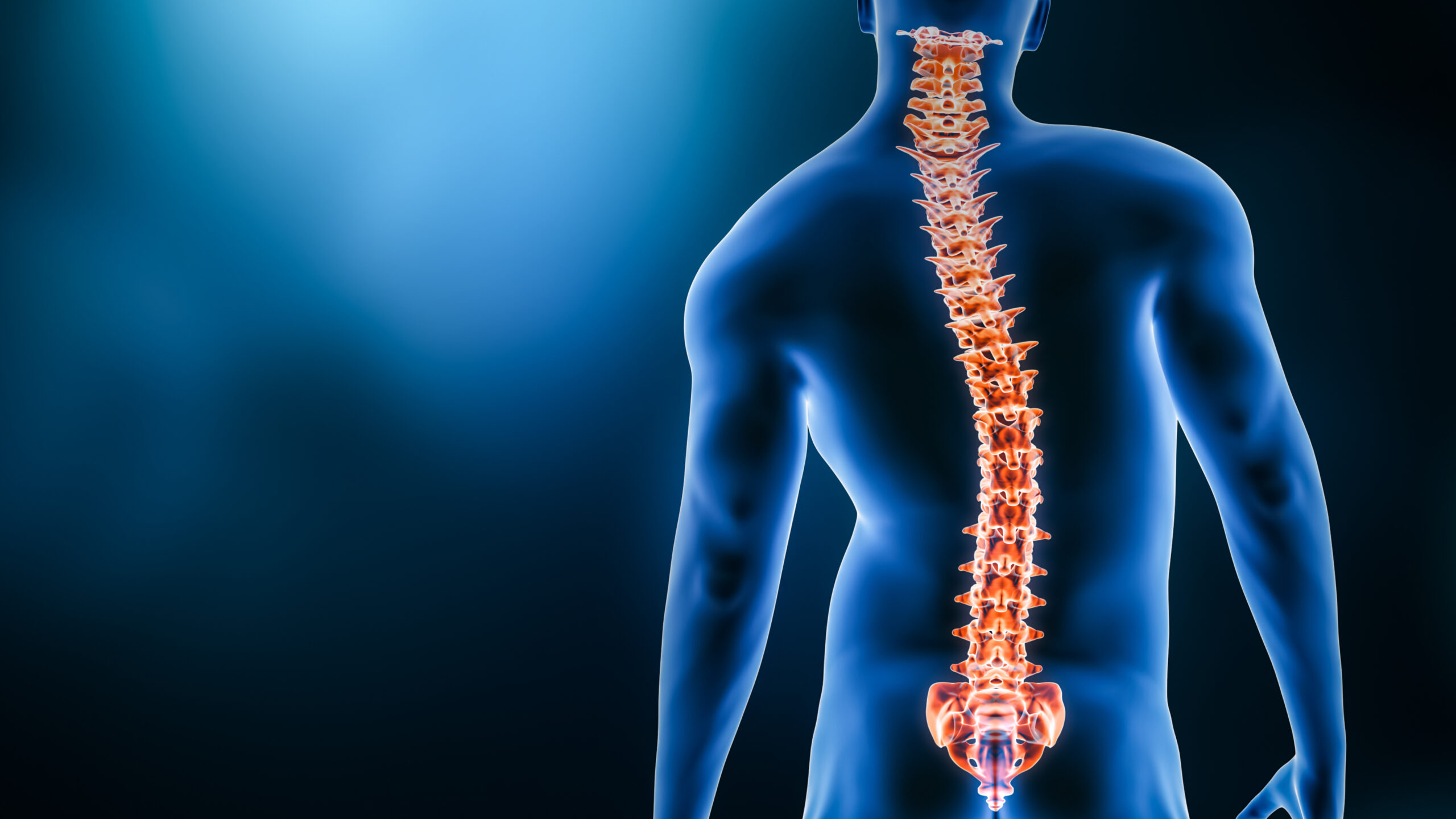
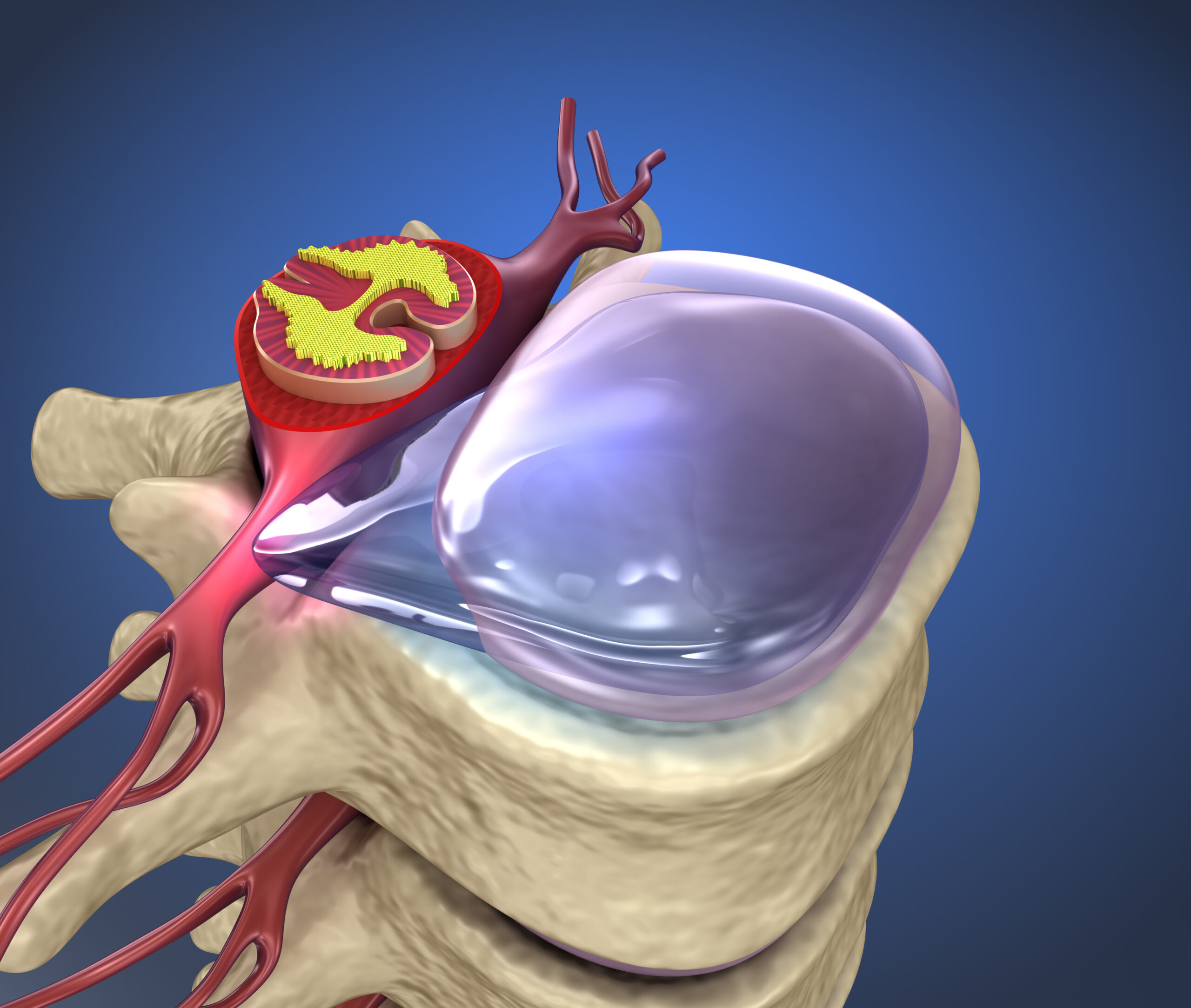
Spinal Manipulation: This technique involves applying pressure to the affected area, using hands or specialized instruments, to realign the joint and alleviate the pain. The chiropractor will use quick, controlled movements to move the joint into its proper position. The goal of spinal manipulation is to restore joint mobility and reduce inflammation.
Stretching and Strengthening Exercises: The chiropractor may recommend specific exercises that target the muscles supporting the sacroiliac joint. These exercises help to improve flexibility, strength, and stability, reducing the risk of future injury.
Soft Tissue Therapy: The chiropractor may use soft tissue therapy to relieve muscle tension, inflammation, and pain. This technique involves applying pressure to the soft tissues surrounding the joint, using massage, trigger point therapy, or instrument-assisted therapy.
Ultrasound Therapy: This non-invasive technique uses high-frequency sound waves to promote tissue healing and reduce inflammation. The chiropractor will apply a small device over the affected area, and the waves will penetrate the tissues, increasing blood flow and promoting healing.
In conclusion, sacroiliac joint pain can be a debilitating condition that affects daily life. Chiropractors have several techniques to address the issue, including spinal manipulation, stretching and strengthening exercises, soft tissue therapy, and ultrasound therapy. A personalized treatment plan will be designed based on the individual’s needs and preferences. Chiropractic care can provide an effective, non-invasive solution to sacroiliac joint pain, helping patients to regain their mobility and improve their quality of life.