Low back pain is one of the most prevalent chronic conditions world-wide, affecting adults as young as 18, and worsens with age [4]. Typical interventions for alleviating low back pain involve adjustments in life-style factors such as workload, social support, and physical therapy, with very rare cases requiring admission to an emergency room [2]. However, severe back pain can also be a symptom of a lesser known or misdiagnosed condition [3][4]. For instance, Cauda Equina Syndrome (CES) is a rare condition that typically requires immediate surgical treatment in order to avoid serious excretory complications (incontinence) and permanent nerve damage [5][7].
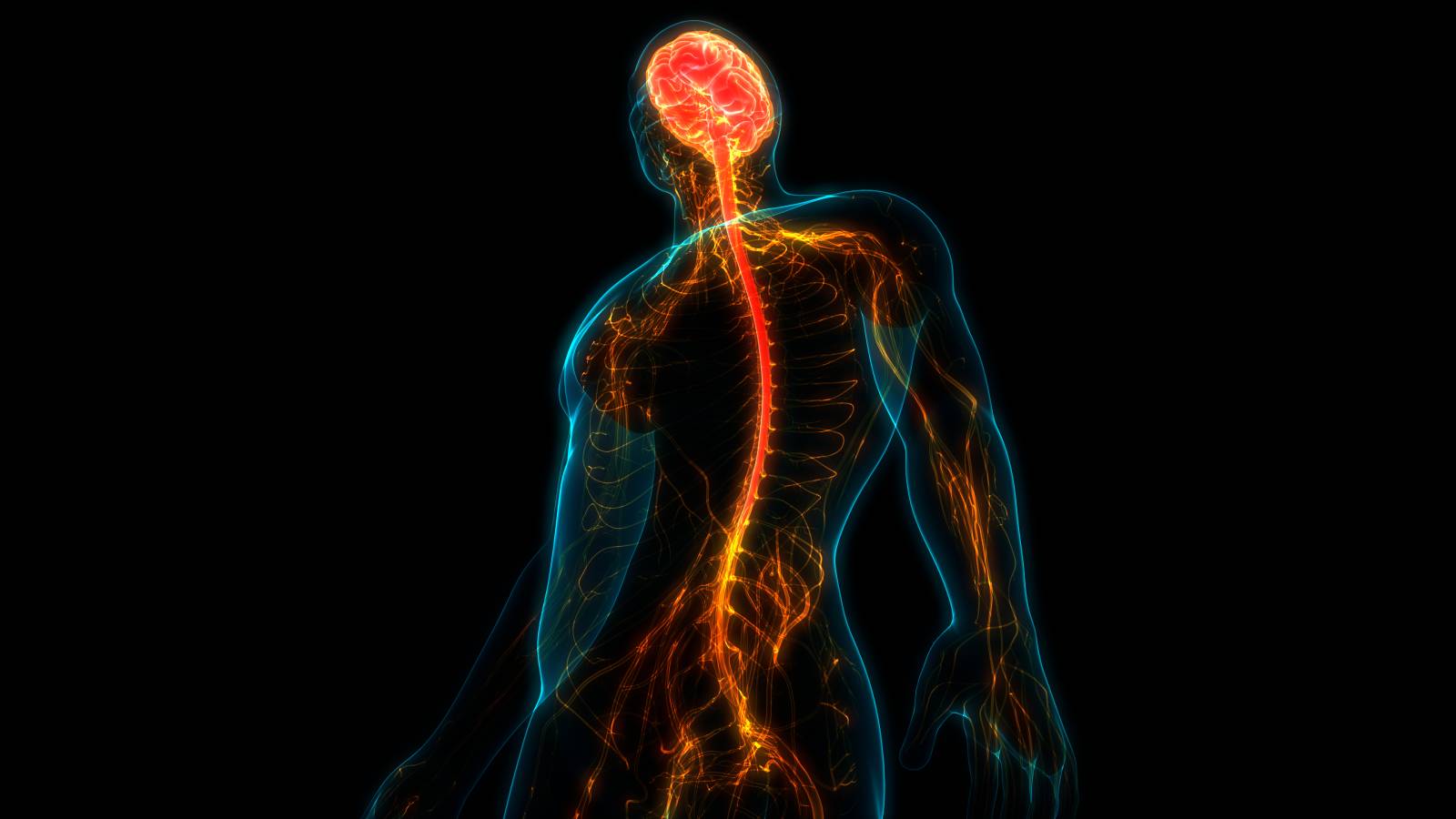
The cauda equina, Latin for “horse’s tail”, is a bundle of spinal nerve roots originating near the distal end of the spinal cord that send and receive nerve impulses to pelvic organs and lower limbs [3][4][7]. Damage to the cauda equina can result in sudden and severe symptoms that disrupt motor and sensory functions of the lower extremities, bladder and bowels [3][5]. Typically, this damage arises from compression and inflammation of the nerve roots, caused by a herniated disc in the lumbar region [3][7]. Common causes of a lumbar disc herniation include excessive pressure from loading or strain from sudden twisting movements [6]. Other causes include but are not limited to spinal infections and inflammation, lumbar spine trauma, spinal lesions and tumors, lumbar spinal stenosis, and spinal hemorrhages [5][7].
The severity of symptoms varies depending on the degree of compression and number of nerves injured [5][6]. For some patients, the onset of cauda equina symptoms can develop within 24 hours (acute onset) or over weeks and months (gradual onset) [5]. Typical symptomatic indicators of CES include severe low back pain, weakness, tingling, or sharp, hot pain in one or both legs and/or “saddle region” (groin, buttocks, genitals, upper thighs), recent onset of bladder and bowel dysfunction and/or incontinence, and loss of reflexes in the lower extremities [3-7]. Patients are typically classified into two categories: CES-R (urinary retention) and CES-I (an incomplete syndrome) [4]. In addition to a diagnostic screening with an MRI, Gardner et al. suggests implementation of a trigone sensitivity test in order to discern “genuine” neurological deficits of bladder retention [4].
As mentioned above, CES usually requires immediate hospitalization and prompt decompression surgery in order to reduce the symptoms of neurological dysfunction and avoid incontinence and permanent paralysis [3][4]. As with most neurological conditions, the sooner the diagnosis and subsequent treatment, the better the chance of recovery with minimal lasting neurological damage [1][4][5]. Ideally, CES is treated early within 24 to 48 hours for the best chance of complete sensory recovery [1][4]. However, surgery does not necessarily eradicate the possibility of irreversible outcomes [6]. It is important to note that the rarity and variability of CES contributes to misdiagnosis and delay of treatment, contributing to its “prominent position in the medico-legal field” [4]. While attention of CES has increased in the medical field, it is crucial for patients and doctors to be informed and aware of this rare syndrome.
References
1. Bečulić, H., Skomorac, R., Jusić, A., Alić, F., Imamović, M., Mekić-Abazović, A., Efendić, A., Brkić, H., & Denjalić, A. (2016). Impact of timing on surgical outcome in patients with cauda equina syndrome caused by lumbar disc herniation. Medicinski Glasnik : official publication of the Medical Association of Zenica-Doboj Canton, Bosnia and Herzegovina, 13(2), 136–141. https://doi.org/10.17392/861-16
2. Buruck, G., Tomaschek, A., Wendsche, J., Ochsmann, E., & Dörfel, D. (2019). Psychosocial areas of work life and chronic low back pain: a systematic review and meta-analysis. BMC musculoskeletal disorders, 20(1), 480. https://doi.org/10.1186/s12891-019-2826-3
3. Cauda Equina Syndrome. American Association of Neurological Surgeons.https://www.aans.org/en/Patients/Neurosurgical-Conditions-and-Treatments/Cauda-Equina-Syndrome
4. Gardner, A., Gardner, E., & Morley, T. (2011). Cauda equina syndrome: a review of the current clinical and medico-legal position. European Spine Journal: official publication of the European Spine Society, the European Spinal Deformity Society, and the European Section of the Cervical Spine Research Society, 20(5), 690–697. https://doi.org/10.1007/s00586-010-1668-3
5. Hoy, D., Bain, C., Williams, G., March, L., Brooks, P., Blyth, F., Woolf, A., Vos, T., & Buchbinder, R. (2012). A systematic review of the global prevalence of low back pain. Arthritis and Rheumatism, 64(6), 2028–2037. https://doi.org/10.1002/art.34347
6. Kapetanakis, S., Chaniotakis, C., Kazakos, C., & Papathanasiou, J. V. (2017). Cauda Equina Syndrome Due to Lumbar Disc Herniation: a Review of Literature. Folia Medica, 59(4), 377–386. https://doi.org/10.1515/folmed-2017-0038
7. Villavicencio, A. Cauda Equina Syndrome (2016). Cauda Equina Syndrome. Spine-Health. https://www.spine-health.com/conditions/lower-back-pain/cauda-equina-syndrome